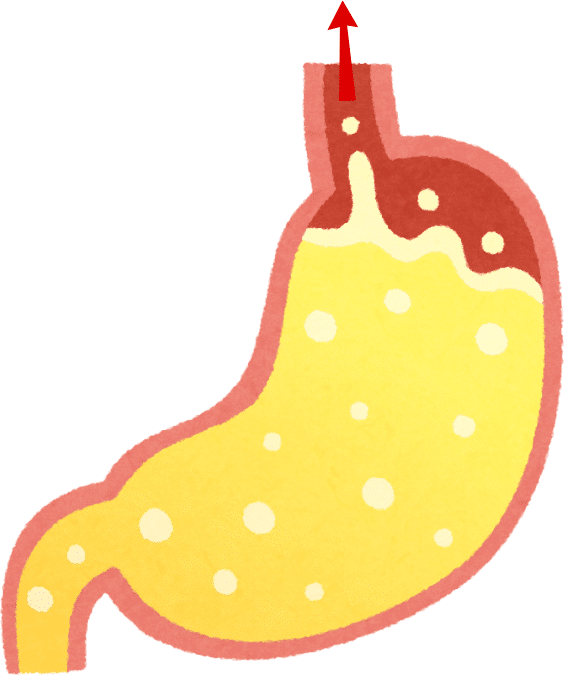
Reflux comes from Latin “refluxus” and means backflow.
Gastroesophageal reflux occurs when (acidic) stomach contents flow back into the esophagus. This happens when the sphincter muscle between the esophagus and the stomach does not function properly.
It leads to symptoms such as heartburn, pain in the upper abdomen and chest area, acid reflux and, in some cases, vomiting.
Reflux is exacerbated by eating foods that increase stomach acid production, such as spicy or fatty foods.
In addition, lying flat or high intra-abdominal pressure can physically increase reflux. If acidic stomach contents are allowed to flow back into the esophagus over a longer period of time, this can irritate the esophagus and lead to painful inflammation of the esophageal mucosa (reflux esophagitis).
Diagnosis
If there are typical symptoms, the condition can be confirmed by gastroscopy or by measuring the pH values of the esophagus and stomach.
Therapy
Home remedies such as sitting upright after eating, no consumption of foods that stimulate additional acid production in the stomach.
Medical therapy with “acid blockers” (proton pump inhibitors). These are drugs that reduce acid production in the stomach (e.g. omeprazole or pantoprazole). This usually helps the affected children quickly and effectively, although it should be noted that children with this condition usually require an increased dose.
Surgically through a Nissen fundoplication. This involves forming a type of sleeve from the upper stomach area, which is placed around the lower end of the esophagus to support the sphincter muscle.
The Situation With PCH2 Children
Children with PCH2 often experience increased vomiting and gastroesophageal reflux. According to many parents, this leads to a severely reduced quality of life due to the children’s discomfort and pain.
PCH2 children cannot express their symptoms to us directly.
The parents often recognize reflux symptoms in the form of severe restlessness and hyperextension, crying and an acidic smell when burping, and obvious signs of pain in their children, who do not respond to the usual painkillers.
As the symptoms (and secondary conditions) of gastroesophageal reflux can often be treated relatively easily using the above-mentioned medications, sparing children pain in the process, parents and doctors of children with PCH2 should be mindful of this condition early on and treat it if necessary.
However, some special dosage considerations must be made (see tips and literature sections). Many parents consider the proton pump inhibitor omeprazole to be one of the key drugs in the treatment of the symptoms of PCH2.
Tips to Try Out
- Avoid foods that stimulate stomach acid production (spicy food, very hot or cold food, fatty foods).
- Sit upright for 30 minutes after eating.
- For children with PEG tubes: de-airing of the stomach via the tube
- Consider gastroesophageal reflux early on if the child’s symptoms are unclear and initiate medical treatment if necessary (make sure the dosage is sufficiently high and adjust the dose as the child grows!)
! Treatment with significantly higher doses of proton pump inhibitors has proven to be effective: 3-5 mg/kg bw, divided into several doses daily.
Scientific Background
Data From Literature
- Andersson et al. (2000) investigated the pharmacokinetics of orally administered omeprazole (a proton pump inhibitor) in children with esophagitis and reflux. They found that younger children in particular require higher doses of omeprazole per kilogram of body weight than adults.
- Böhmer et al. (1997) found that people with mental disabilities often develop reflux esophagitis. Other risk factors mentioned in the study were cerebral palsy, an IQ below 35, scoliosis and the use of anticonvulsant medication or benzodiazepines. For suspected reflux, early diagnostic confirmation by means of endoscopy or 24h-pH-metry is recommended and reference is made to the highly effective, symptom-relieving and positive effect on quality of life of treating with proton pump inhibitors.
- In a subsequent study, Böhmer et al. (1998) suggest that omeprazole is a highly effective drug for the treatment of reflux disease in children with mental impairment.
- Hassall et al. (2000) confirmed the high efficacy, good tolerability and safety of omeprazole for the treatment of erosive esophagitis and gastroesophageal reflux in children, even in cases where antireflux surgery or other medical therapies had previously failed. This study reiterates that the required doses per kilogram are higher in children than in adults.
Natural History Study from 2014
In total, 31 out of 33 children experienced increased vomiting. In 23 cases, gastroesophageal reflux was diagnosed by a doctor. A total of 17 study participants received long-term therapy with proton pump inhibitors. Fundoplication was performed in 12 children.
Natural History Study from 2023
Of 53 children, 48 showed symptomatic reflux, which started on average at the age of one year according to the parents. The formal diagnosis of “gastroesophageal reflux” was given to 25 of these 48 children. All children who, according to their parents, did not show signs of reflux in the study were younger than 2 years at the time of data collection. In 7 cases, children no longer experienced reflux as the study progressed; in 5 cases, the parents associated this with fundoplication.
43 children were treated with a proton pump inhibitor (mostly omeprazole). The children received a median dosage of 3.1 mg/kg bw divided into 3 doses daily. 34 parents stated that they considered the proton pump inhibitor to be one of the key medications for their children and that it had led to significantly improved symptoms such as crying, reflux, restlessness and vomiting.
This entry was written to the best of our knowledge based on the reported experiences of parents of affected children. In addition, currently available data from the 2014 and 2023 Natural History Studies of PCH2 and from general medical literature has been included. It is not a substitute for consulting a medical professional. PCH2cure assumes no liability in this respect.
- Andersson T, Hassall E, Lundborg P, Hirte R, Radke M, Marcon M, Dalväg Ein, Martin S, Behrens R, Koletzko S, Becker M, Drouin E, Göthberg G (2000) Pharmacokinetics of orally administered omeprazole in children. International Pediatric Omeprazole Pharmacokinetic Group. Bin J Gastroenterol. 95(11):3101-6.
- Böhmer CJ, Niezen-de Boer MC, Klinkenberg-Knol EG, Tuynman HA, Voskuil JH, Devillé WL, Meuwissen SG (1997) Gastroesophageal reflux disease in intellectually disabled individuals: Leads for diagnosis and the effect of omeprazole therapy. Bin J Gastroenterol. 92(9): 1475-9.
- Böhmer CJ, Niezen-de Boer MC, Klinkenberg-Knol EC, Nadorp JH, Meuwissen SG (1997) Gastro-oesophageal reflux disease in institutionalised intellectually disabled individuals. Neth J Med. 51(4):134-9.
- Böhmer CJ, Niezen-de Boer RC, Klinkenberg-Knol EC, Neuwissen SG (1998) Omeprazole: Therapy of choice in intellectually disabled children. Arch Pediatr Adolesc Med. 152(11): 1113-8.
- Hassal E, Israel D, Hirte R, Radke M, Dalväg Ein, Sköld B, Junghard O, Lundborg P (2000) Omeprazole for treatment of chronic erosive esophagitis in children: a multicenter study of efficacy, safety, tolerability and dose requirements. International Pediatric Omeprazole Study Group. J Pädiatr. 137(6): 800-7.
- Natural History Study from 2014: Frölich S. Natürlicher Verlauf der Pontocerebellären Hypoplasie Typ 2 [Dissertation to Acquire the Academic Degree Doctor of Medicine] Tübingen: Eberhard-Karls-Universität; 2014.
- Natural History Study from 2023: Kuhn A L. Gastrointestinale Symptome, Ernährung und Gedeihen bei Pontocerebellärer Hypoplasie Typ 2 A [Dissertation to Acquire the Academic Degree Doctor of Medicine] Freiburg im Breisgau: Albert-Ludwigs-Universität; 2023.